Latest videos


SUPPORT/JOIN THE CHANNEL: https://www.youtube.com/channe....l/UCZaDAUF7UEcRXIFvG
My goal is to reduce educational disparities by making education FREE.
These videos help you score extra points on medical school exams (USMLE, COMLEX, etc.)
For educational purposes only; NOT medical or other advice.
Some videos contain mild profanity and hyperbole solely used to assist with memorization. Viewer discretion advised.
Opinions are entirely my own.


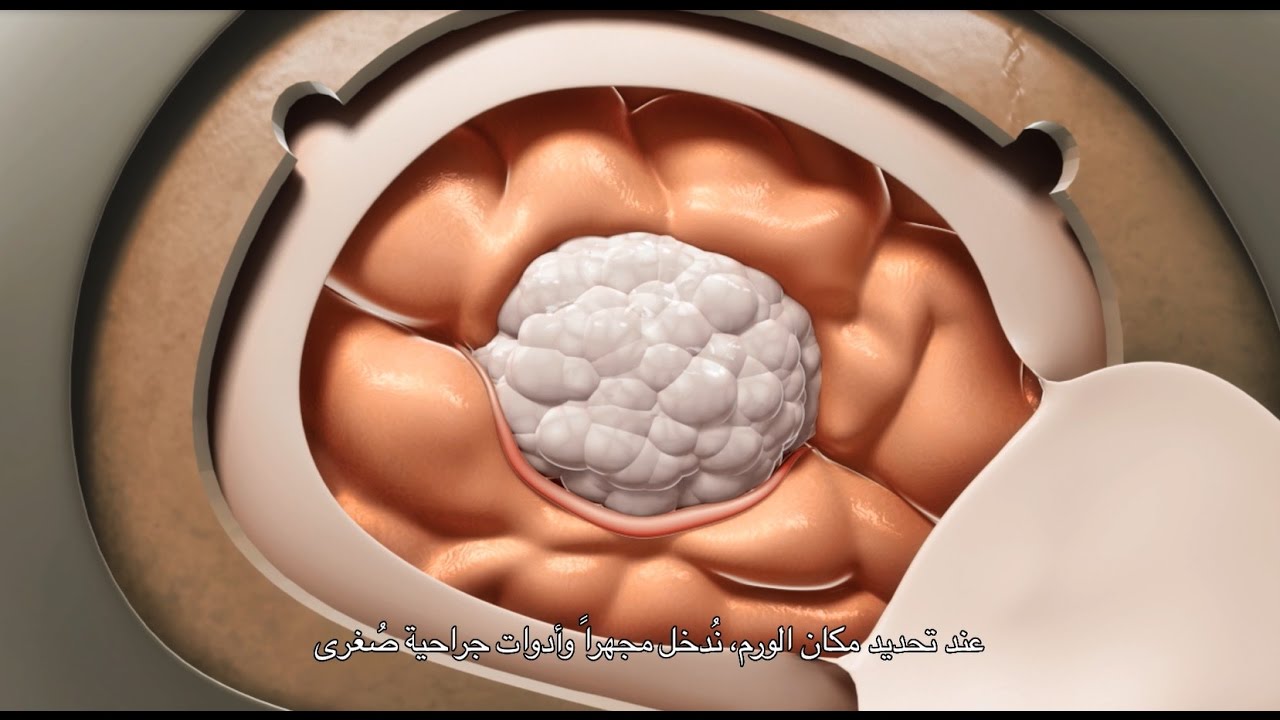
Susan Rooney was diagnosed with a brain tumor days before her daughter’s high school graduation. It was stage 4, generally considered incurable. After surgery and chemotherapy proved ineffective, Rooney joined a clinical trial testing a new drug – one of several leading edge therapies offered at Moores Cancer Center at UC San Diego Health. Today, the tumor is stable and under control and Rooney is again enjoying life.
Learn more about comprehensive brain tumor treatment at UC San Diego Health: https://health.ucsd.edu/specia....lties/cancer/program


Diagnosed with a grade two astrocytoma brain tumor, Carlos Luceno is currently living with brain cancer. Carlos is receiving his treatment and care from Johns Hopkins neurosurgeon Dr. Henry Brem at the Johns Hopkins Comprehensive Brain Tumor Center. Learn more about the Johns Hopkins Comprehensive Brain Tumor Center http://www.hopkinsmedicine.org..../neurology_neurosurg
For appointments, Maryland residents should call 410-955-6406, and out-of-state residents should contact 1-855-884-6754.