Video terbaru


Diagnosed with a rare spinal cord tumor known as a hemangioblastoma, Bridget sought treatment from the experts at Johns Hopkins Medicine. Middle schooler Bridget is an avid soccer player, but she and her family members noticed she was experiencing weakness, numbness and loss of coordination in her right leg. Pediatric neurosurgeon Mari Groves successfully removed the #SpinalCordTumor, and Bridget received rehabilitation at the Kennedy Krieger Institute. Bridget also had genetic testing at #JohnsHopkins due to a family history of spinal cord lesions. Bridget is now symptom-free and enjoying her active life.
For more information, visit https://www.hopkinsmedicine.org/pedsneurosurgery


This webinar was recorded on May 28th. An overview of the treatment of pediatric low grade gliomas. The webinar features Mayo Clinic Pediatric Neurosurgeon, David Daniels, MD and Mayo Clinic Pediatric Neurologist, Gesina Keating, MD. Both physicians will discussed diagnosis and treatment options including: observation, surgery and chemotherapy. Follow-up care for pediatric low grade gliomas including: Pilocytic Astrocytomas, Gangliogliomas, DNETs and other low grade brain tumors. After the presentation Dr. Daniels and Dr. Keating participated in a live question and answer session.
To join the discussion and ask a question: http://mayocl.in/1zkzCjT


Symptoms, risk factors and treatments of Pilocytic astrocytoma (Medical Condition)
A WHO grade I, generally well circumscribed, slowly growing, often cystic astrocytoma
This video contains general medical information If in doubt, always seek professional medical advice.
The medical information is not advice and should not be treated as such. The medical information is provided without any representations or warranties, express or implied. We do not warrant or represent that the medical information on this websiteis true, accurate, complete, current or non-misleading
Music: 'Undaunted' Kevin Macleod CC-BY-3.0
Source/Images: "Pilocytic astrocytoma" CC-BY-2.5 https://www.freebase.com/m/08plh5


🌟 Read More: https://addon.life/2021/04/06/....3-foods-to-avoid-die
No two cancers are the same and neither should your nutrition be. The most commonly asked question to dieticians and oncologists globally is “What Should I Eat?”. The answer is “It Depends”. It depends on the type of cancer, current treatment and supplements being taken, age, gender, BMI, lifestyle and any genetic information available. In short – the answer to “What Should I Eat” for Pilocytic Astrocytoma needs to be personalized to minimize adverse interactions between nutrition (from foods/diet) and treatment, and to improve symptoms.
Foods like Blueberry and Cabbage should be eaten when undergoing Temozolomide treatment for Pilocytic Astrocytoma. On the other hand, for Pilocytic Astrocytoma, Cinnamon and Cowpea should be eaten with treatment of Radiation. On the same lines, foods like Buttermilk and Chili Pepper should be avoided with treatment of Temozolomide for Pilocytic Astrocytoma. If the treatment is Radiation, then avoid Amaranth and Barley.
You get the point – your nutrition needs to be personalized and it needs to be re-evaluated as soon as any of the conditions change. Create and follow a nutrition plan personalized to you to minimize adverse interactions of nutrition for cancers like Pilocytic Astrocytoma.
https://addon.life/onboarding/
☝ Create Personalized Nutrition Plan for Cancer
✅ Facebook: https://www.facebook.com/addonForCancer/
✅ Twitter: https://twitter.com/addonForCancer/
✅ Instagram: https://www.instagram.com/addonForCancer/
✉ Email: nutritionist@addon.life | © Copyright 2021, addon.life.

Brain tumors are one of the most common diagnoses addressed in neuroradiology. This covers a wide spectrum of disease, from primary brain tumors like gliomas and glioblastomas to secondary disease like metastases. This lecture covers the spectrum of the most common brain tumors, with an emphasis on primary brain tumors.
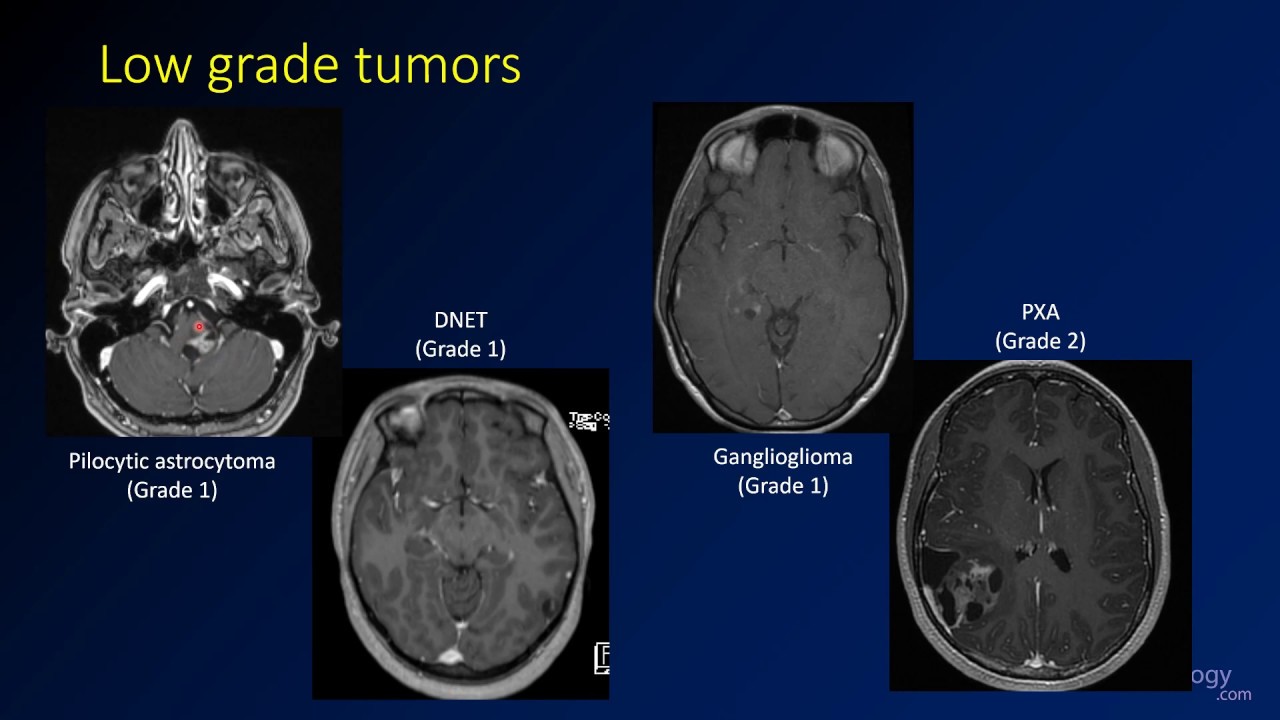
This video discusses imaging and genetic features of some less common low grade tumors like pilocytic astrocytoma, dysembryoplastic neuroepithelial tumor (DNET), ganglioglioma, and pleomorphic xanthoastrocytoma (PXA). These tumors are often seen in younger patients, many of whom will present with seizures. Surgery is often curative. There is a lot of imaging overlap for these tumors, especially DNET and ganglioglioma, which can appear very similar. However, the specific diagnosis is less important than knowing that a lesion may be a low grade glioma.
Additional videos in the playlist will address the imaging findings of other types of brain tumors.
The level of this lecture is appropriate for radiology residents, radiology fellows, and trainees in other specialties who have an interest in neuroradiology or may see patients with brain tumors.
Check out this video and additional content on http://www.learnneuroradiology.com


📌 𝐅𝐨𝐥𝐥𝐨𝐰 𝐨𝐧 𝐈𝐧𝐬𝐭𝐚𝐠𝐫𝐚𝐦:- https://www.instagram.com/drgbhanuprakash
📌𝗝𝗼𝗶𝗻 𝗢𝘂𝗿 𝗧𝗲𝗹𝗲𝗴𝗿𝗮𝗺 𝗖𝗵𝗮𝗻𝗻𝗲𝗹 𝗛𝗲𝗿𝗲:- https://t.me/bhanuprakashdr
📌𝗦𝘂𝗯𝘀𝗰𝗿𝗶𝗯𝗲 𝗧𝗼 𝗠𝘆 𝗠𝗮𝗶𝗹𝗶𝗻𝗴 𝗟𝗶𝘀𝘁:- https://linktr.ee/DrGBhanuprakash
Gliomas (Neurology) : Expert Talk by Dr. Krishna Kumar ( Consultant Neurosurgeon )
Gliomas account for the great majority of primary tumors that arise within the brain parenchyma. The term "glioma" refers to tumors that have histologic features similar to normal glial cells (ie, astrocytes, oligodendrocytes, and ependymal cells). For each of these types of gliomas, there are neoplasms that span a broad spectrum of biological aggressiveness.
Historically, the slower-growing lesions, corresponding to World Health Organization (WHO) grades I and II, have been commonly referred to as low-grade gliomas, while the more rapidly progressive tumors are referred to as high-grade gliomas. The WHO classification recommends avoiding these terms since they lump together heterogeneous groups of tumors, many of which have significantly different biologic properties, prognoses, and treatment approaches. Among grade I and grade II gliomas, for example, current classification favors a distinction between diffuse gliomas (eg, grade II diffuse astrocytoma and oligodendroglioma) and more circumscribed astrocytic tumors (eg, grade I pilocytic astrocytoma). Additionally, it is clear that among grade III and grade IV tumors, there can be markedly different courses, including responses to therapies.
#gliomas #gliomasneurology #gliomaspatienteducation #gliomaseverythingyouneedtoknow #gliomasexperttalk #gliomaslecture #gliomasneurosurgery #gliomasvideo #braintumor #braintumorsurgery #gliomasneuropathology





