Последние видео


Dr. Daniel Kelly, Director of the Pacific Pituitary Disorders Center, Pacific Neuroscience Institute, demonstrates the technique of endonasal endoscopic removal of a pituitary macrodenoma. The methods of tumor resection, pituitary gland preservation, skull base closure and CSF leak repair are shown.
Endoscopic surgery for pituitary macroadenomas has been shown to be very efficacious for maximal tumor resection. Over the last decade, this technique has become the preferred method for removal of the great majority of pituitary adenomas and has been shown to be associated with very high degrees of tumor resection and gland preservation. Non-functional (non-secreting) pituitary macroadenomas, typically cause vision loss (typically peripheral vision), pituitary dysfunction and headaches.
At the Pacific Pituitary Disorders Center, we have one of the world's largest experiences in endonasal endoscopic surgery and comprehensive care for patients with pituitary adenomas and related skull base tumors.
https://pacificneuro.org
https://pacificneuro.org/kelly
https://pacificpituitary.org | 310-582-7450


Dr. Daniel Kelly, Pacific Neuroscience Institute, Founder and world-renowned Neurosurgeon talks about the state of the art endoscopic endonasal pituitary surgery and the team approach PNI takes for treating patients with pituitary adenomas (tumors).
Given the complexity of pituitary adenomas and the impact on hormonal function, vision, general health, and the location in the skull base, a multidisciplinary team approach, consisting of neurosurgeons, endocrinologists, neuro-ophthalmologists, radiation oncologists, otolaryngologist, neuroradiologist. is essential for optimal outcomes and pituitary tumor care.
https://www.pacificneuroscienc....einstitute.org/pitui
310-582-7450
#pituitarytumor
#pacificneuro

This video is no longer up to date, watch the new version of this video:
https://youtu.be/UUb_pRr4jnk
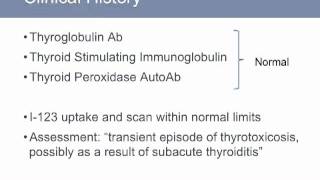
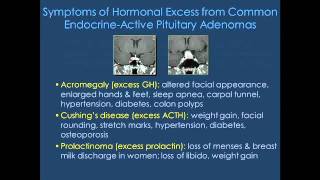
http://newstjohns.org/BTC_Con_....Pituitary_Tumors_And
Pituitary Gland disorders and tumors can be very challenging to diagnose and treat. In this video, Dr. Daniel Kelly, Director of the Saint John's Brain Tumor Center & Pituitary Disorders Program discusses the essential hormonal functions of the pituitary gland, its anatomy in relation to the surrounding skull base and brain, and the wide-ranging effect of pituitary adenomas and related tumors which may include hormonal abnormalities, visual loss and headaches. The pituitary gland is known as the master gland, because it regulates the function of the great majority of endocrine glands throughout the body. These functions include regulating the body's stress response (through adrenocorticotropic hormone -- ACTH), metabolism (through thyroid stimulating hormone -- TSH), tissue and bone growth (through growth hormone -- GH), sexual function and reproduction (through luteinizing hormone -- LH and follicular stimulating hormone -- FSH), breast feeding and milk production (through prolactin & oxytocin), and water and electrolyte balance (through vasopressin also known as antidiuretic hormone -- ADH). Pituitary tumors and cysts can cause pituitary gland dysfunction by compressing the gland affect its various functions. Symptoms of pituitary hormonal dysfunction (under-production) include fatigue, decreased energy, weight gain, light-headedness, growth delay (in children), infertility, sexual dysfunction, increased urination and increased thirst, to name a few. The most common pituitary tumors are pituitary adenomas of which there are two major categories. Endocrine-active pituitary adenomas produce excess hormones and include those causing acromegaly from excess GH, Cushing's disease from excess ACTH, prolactinomas from excess prolactin and the rare TSH-secreting adenomas. In contrast, endocrine-inactive adenomas do not produce excess hormones and typically cause symptoms of "mass effect" which may include hormonal loss (hypopituitarism), visual loss, headaches and tumor bleeding (pituitary apoplexy). The other common tumors that may arise in the region of the pituitary gland include craniopharyngiomas, Rathke's cleft cysts, meningiomas and clival chordomas. This video provides a brief description of all these tumor types. Given the complexity of diagnosing and optimally treating pituitary tumors and related hormonal disorders this video also stresses the importance of a multidisciplinary approach to evaluating and treating pituitary patients that includes neurosurgeons, otolaryngologists (ENT surgeons), endocrinologists, neuro-ophthalmologists, radiation oncologists, neuro-pathologists and neuro-radiologists. The great majority of symptomatic pituitary tumors will warrant treatment with endonasal endoscopic surgery although prolactinomas can typically be treated with dopamine agonist medical therapy. At the Saint John's Brain Tumor Center and Pituitary Disorders Program, we have one of the world's largest experiences in endonasal endoscopic surgery and comprehensive care for pituitary adenomas and related tumors.


To learn more about pituitary tumors, please visit https://cle.clinic/3orsfbG
Pituitary tumors start in the pituitary gland. They’re usually benign (not cancerous) and rarely spread to other parts of the body. Dr. Borghei-Razavi discusses pituitary tumors and treatments through minimally invasive surgical approaches offered at Cleveland Clinic Florida.
▶Share this video with others:
▶Subscribe to learn more about Cleveland Clinic: https://www.youtube.com/user/C....levelandClinic?sub_c


Visit https://mayocl.in/2TxGyhY for more information on pituitary tumor care at Mayo Clinic or to request an appointment.
Jamie J. Van Gompel, M.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota, and Irina Bancos, M.D., an endocrinologist at Mayo Clinic's campus in Minnesota, discuss pituitary tumors that produce growth hormone. Pituitary tumors are common and often don't cause problems. But some pituitary tumors secrete growth hormone — leading to a syndrome that's characterized by soft tissue growth and swelling (acromegaly).
Dr. Bancos notes that acromegaly develops very slowly and is often overlooked. She outlines the syndrome's indications, including coarsened facial features and changes in shoe size. Dr. Van Gompel explains the importance of timely treatment to halt acromegaly. Minimally invasive or open surgery to remove the tumor is often recommended. Treatment might also involve medication or radiation therapy or both.
Dr. Van Gompel provides an overview of the various types of surgery and radiation therapy that are available.


In this video, neurosurgeon Eze Goldschmidt, MD, PhD and head & neck cancer surgeon Ivan El-Sayed, MD perform an endonasal endoscopic resection of a cystic pituitary adenoma in a 58-year-old man who presented with severe vision loss. The MRI revealed a large sellar mass, which was diagnosed as a pituitary adenoma.
“The endoscope allowed us to see the entire extension of the tumor,” Goldschmidt said. “We first removed the calcified parts, then dissected the tumor from the cavernous sinus and removed it completely to decompress the optic chiasm.”
The patient’s vision returned to normal after the surgery, and a postoperative MRI showed complete removal of the lesion.
“Pituitary adenomas are relatively common,” Goldschmidt said. “We have removed many of them using the endonasal approach.”
For more information about Dr. Ezequiel Goldschmidt, MD, PhD, visit: https://www.ucsfhealth.org/pro....viders/dr-ezequiel-g
To contact UCSF Health's physician's referral services, visit: https://www.ucsfhealth.org/for....-health-professional